Milton N Moraes-Filho 1,2, Adriana Berezovsky1, Rubens Belfort Jr. 1, Solange R. Salomão 1
1 Departamento de Oftalmologia e Ciências Visuais, Escola Paulista de Medicina, Universidade Federal de São Paulo – UNIFESP, São Paulo, SP, Brasil
2 Instituto de Olhos de Colatina, Colatina, ES, Brasil
Differential diagnosis between toxic and/or nutritional etiologies for LHON cases must be considered when symmetric acute or subacute visual loss and/or color vision defect is detected.
Three brothers with 11778 mtDNA mutation genotype will be presented: one with classical disease and the others with late onset. They were all exposed to toxic agents that may contribute to bilateral papillomacular bundle damage. One of them showed spontaneous visual recovery after smoking cessation.
Case 1 (VC): Classic LHON
A male was examined between 2001 and 2004, with a past ocular history of acute visual blurring and loss of color vision (around days), nearly his 27 years of age. The vision loss was asymmetric, with an interval of around 6 months between eyes, associated with ocular pain and headache.
He was a heavy smoker (about 1 pack of homemade cigarettes/day) from the age of 12 years. When visual symptoms were felt he was smoking 15 cigarettes/day. He reported no alcohol consumption at visual symptoms onset. However, on 2001, the alcohol consumption was 4 doses of cachaça (sugar cane spirit)/weekend. The patient quit smoking at 51 years of age (on 2003). His occupation was agricultural worker and he was exposed once to a pesticide spray (with the anticholinesterase compound named Omethoate in the formula). No dietary deficit was detected. However, his body mass index (BMI) was 17.3 Kg/m2 (underweight).
The Figure 1 (A) shows severe bilateral diffuse optic nerve atrophy, cup/disk ratio 0.8-0.9 OD and 0.8 OS (deep cup) and normal macula OU. Pupillary reflexes were sluggish light reactive, but no afferent pupillary defect was detected. The retinal nerve fiber layer (RNFL) measurement by polarimetry (GDx) showed a profound RNFL thickness decrease in OU (Figure 1, B).
Visual acuity was hand movements in OU and therefore no visual field testing was performed. The intraocular pressure was 16/18 mmHg, respectively. Thus, suspicion of Low Tension Glaucoma with LHON was raised. Timolol maleate 0,5% bid was prescribed in OU since 2001. No fundus or visual acuity changes up to the last follow up were detected (2004).
The histopathology corroborates the clinical findings. showing intense depletion of axonal fibers, with remaining axons at far nasal periphery (Figure 1, C).
Case 2 (VJC): tobacco-alcohol amblyopia /LHON
This patient was firstly examined at 56 years old (2001). His vision loss occurred when he was 51 years old. It reported progressive bilateral symmetric dimming and loss of colors, lasting about 2 years. He had no alcohol consumption at disease presentation. However, the behaviour for drinking began since his vision dropout (about 4 doses of cachaça/weekends).
The patient was a heavy smoker (about 1 pack of cigarettes/day), from the age of 13 years. No dietary deficiency was reported or detected, including at time of visual loss. Also, his body mass index (BMI) at 56 years old was normal (18.5 kg/m2).
The peasant was exposed to formicides Arsenic and Blenco® for 20 years (twice a month), before the loss of vision. The latter was a liquid used to fill into the anthill and fired, followed by an explosion of Methyl Bromide gas (highly toxic). The methyl bromide can cause bilateral visual loss, temporal ONH pallor, and a severe deuteranomalous (green) defect (Chavez CT et al, 1995).
A papillomacular bundle loss was detected in both eyes at the first examination (Figure 2, A). Concomitant progressive vision loss and smoking/drinking custom in the following years were reported and more severe optic disc pallor was detected at last examination (2004).
The patient had arterial hypertension and essential tremor as. He died by acute myocardial infarction. Histopathology of the optic disc showed atrophy of temporal fibers in OU (Figure 2, D).
Case 3 (AC) tobacco-alcohol amblyopia /LHON
This patient had 13 years of follow up (2001-2014). He was visited for the fist time at the age of 55 years and he claimed visual loss from the age of 42 years. A chronic progressive simultaneous visual blurring and color vision defect with no other associated visual symptoms was reported. Associated co-morbidities were hepatic cirrhosis (diagnosed at the age of 50 years old) and arterial hypertension.
He has been a heavy smoker (30 cigarettes/day) during the last 40 years. Nevertheless, he was obligated to stop smoking after suffering a myocardial infarction (MI) at 61 years of age. He also was a heavy drinker for 29 years (5 doses/day), stopped after cirrhosis diagnosis, returned at 58 years old and again stopped for the second time after the MI. No dietary deficiency was detected and the BMI was 34.9 Kg/m2.
In 2001 bitemporal optic disk pallor was detected in both eyes (Figure 3), The intraocular pressure was 15 and 16 mmHg in the right and left eye respectively and no afferent pupillary defect was detected.
A partial visual function (acuity and field) recovery was recorded after smoking cessation (Figure 4). The red free filter image(that emphasizes retinal nerve fiber layer brightness) showed bitemporal loss of bright on the last visit (2014), even with visual recovery after smoking cessation (Figure 3).
Comments
Those three 11778 mtDNA LHON brothers illustrated different features of LHON. The youngest one showed typical and profound loss of axonal fibers, as occurs to the young group (<30 years of age) into the large cohort studied from the Brazilian family (Sadun AA et al, 2003). Meanwhile, the remaining brothers showed mild temporal disk pallor during the cigarette consumption. Curiously, the third patient described herein showed a partial improvement of his vision when giving up smoking.
The tobacco/alcohol amblyopia is characterized by late onset of bilateral visual loss and color discrimination defect, bitemporal optic disk pallor, central or cecocentral visual field defect and papillomacular bundle damage (Grzybowski A et al, 2015). Those clinical features were observed on the oldest LHON brothers.
Carelli et al. (Carelli V et al, 2016) have recently described a second variant of LHON named type II. Differently by the classical type I LHON (as case #1), this subgroup comprises late onset vision loss (> 30 years of age) that might be triggered by external toxic factors, like tobacco abuse (cases #2 and #3).
References:
Carelli V, d’Adamo P, Valentino ML, La Morgia C, Ross-Cisneros FN, Caporali L, et al. Parsing the differences in affected with LHON: genetic versus environmental triggers of disease conversion. Brain 2016;139:e17.
Chavez CT, Hepler RS, Straatsma BR. Methyl bromide optic atrophy. Am J Ophthalmol 1985;99:715-719.
Grzybowski A, Zülsdorff M, Wilhelm H, Tonagel F. Toxic optic neuropathies: an updated review. Acta Ophthalmol 2015;93:402-410.
Sadun AA, Carelli V, Salomao SR, Berezovsky A, Quiros PA, Sadun F, et al. Extensive investigation of a large Brazilian pedigree of 11778/haplogroup J Leber hereditary optic neuropathy. Am J Ophthalmol 2003;136:231-238.
Figure legends
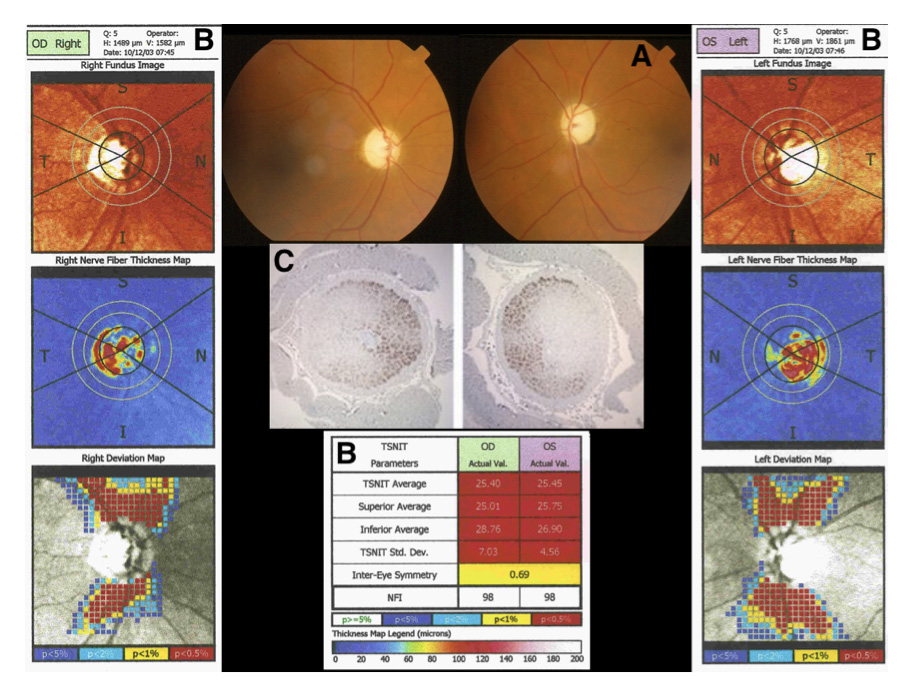
Figure 1. Patient #1, color fundus images (A): severe optic nerve pallor. Polarimetry of the optic nerve disc (B): the retinal nerve fiber layer measurement shows profound thinning in OU. Optic disc histopathology (C): intense depletion of axonal fibers, with remaining axons at far nasal periphery.
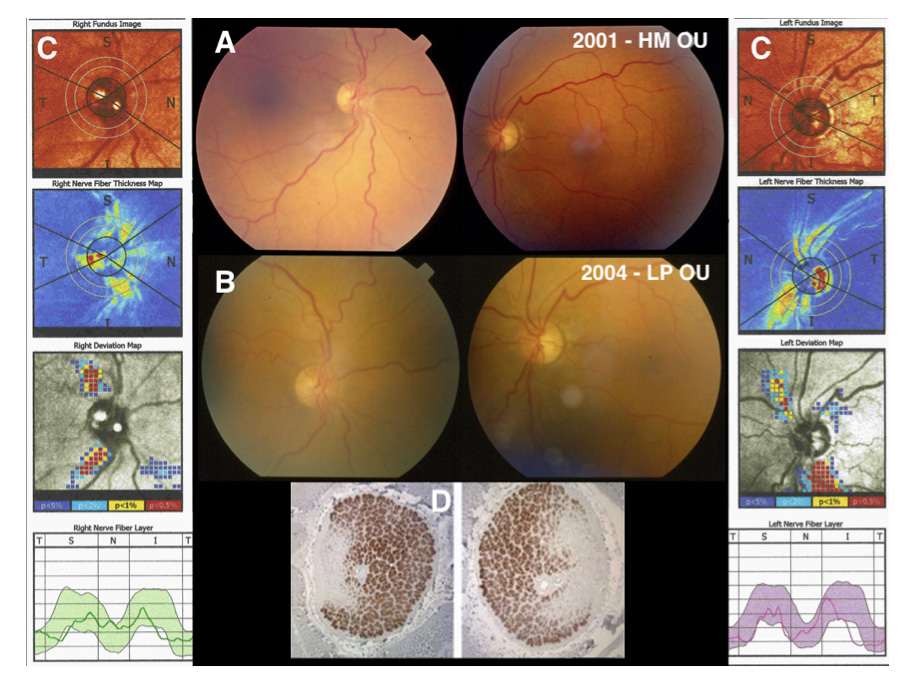
Figure 2. Patient #2, color fundus images (A) 2001: bitemporal optic disk pallor. Color fundus images (B) 2004: bitemporal optic disc pallor. Polarimetry of the optic nerve disc (C) 2001: retinal nerve fiber layer thinning is evident in the thickness map but not in the deviation map. Optic disc histopathology (D) shows atrophy of temporal fibers in OU. HM: hand motion; LP: light perception.
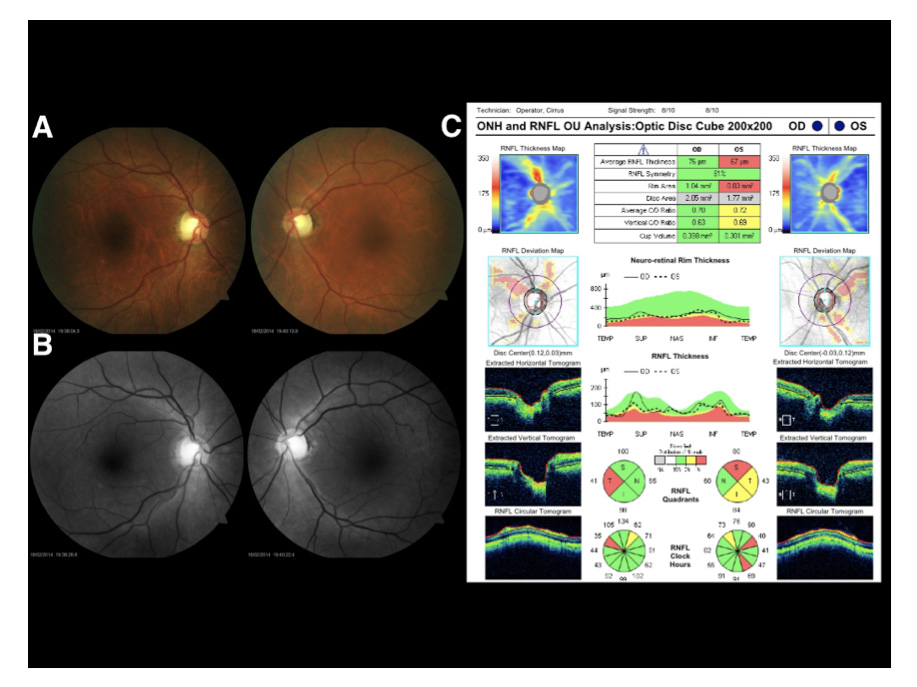
Figure 3. Patient #3, color fundus images (A) 2001: bitemporal optic disk pallor in OU. Red free filter images (B) 2014: bitemporal loss of bright. OCT (C): loss of temporal retinal nerve fiber layer.
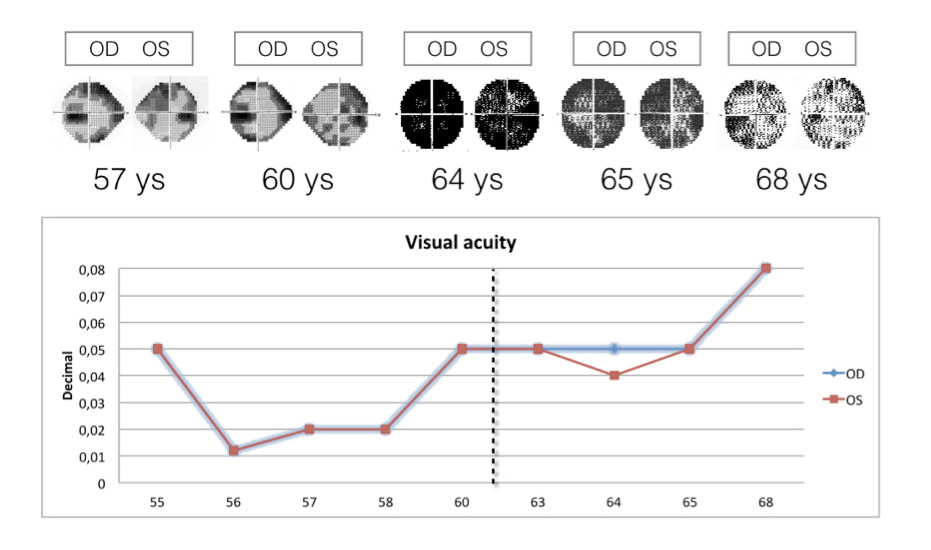
Figure 4. Longitudinal Humphrey visual field and visual acuity changes in patient #3. Note the partial visual function (acuity and field) recovery after smoking cessation (event marked with dotted line).
